This includes the variety of examinations Animal Eye Care performs depending on the individual case.
1. History: discharge, squinting, redness, cloudiness, vision loss, medications
2. Breed Predisposition
3. Observe from a distance: squinting, cloudiness, redness, symmetry
4. Close-up: - menace response (cover each eye in turn), retropulsion of the globes
5. If mucky discharge present, or corneal or conjunctival disease suspected, a Schirmer Tear Test should then be performed before touching/stimulating the eye much. Similarly perform early in the examination for rechecks of dry eye. Place the bent paper strip 2/3 to ¾ way along eyelid towards the lateral canthus for 1 minute. Normal is 15mm/min.
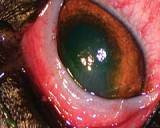
6. (Darkened room) Focal light examination: PLR (direct and consensual), eyelids, conjunctiva, cornea, lens/tapetal reflection. At this point you are trying to localise the lesion. A slit beam can help to locate the depth/position of a lesion (present on many ophthalmoscopes).
7. Magnification e.g. slit lamp, Lumiview (Welch Allyn), head loupe, head torch and 20D lens works well for magnification. Check eyelids (distichia, entropion, tumours), conjunctiva, cornea, iris, lens.
8. Fundus examination: indirect ophthalmoscopy (head torch or focal light, 20D lens), direct ophthalmoscopy (less useful – ophthalmoscope), panoptic.
9. Fluorescein staining: apply with dye impregnated strip – just touch onto conjunctiva once then flush with a few drops of artificial tears. Do not leave excess stain on the cornea.
10. Fluorescein passage through the tear duct. Apply slightly more stain than for corneal staining then a few drops of tears. Stain should be visible at the nostril within 5-10 mins.
11. Tonometry: applanation (Tonopen), Schiotz. For Schiotz tonometry have 3 people. Apply topical anaesthetic to the eye. One holding the animal, second holding the head – nose up. Vet lowers the footplate onto the cornea momentarily 4-5 times with the reading scale pointing to the nurse holding the head. Each time the needle flicks across the person reading the scale reads out the reading. Once 3-4 similar readings are called out, use these to read of the scale on the table to get IOP.
12. Looking behind the third eyelid: apply topical anaesthetic then grasp the third eyelid with a fine pair of mosquito forceps or move with smooth cilia forceps.