Vision in small animals can be assessed through the menace response (also tests CN VII function and can be absent with cerebellar disease without loss of vision), visual placing response (patient held under chest and brought up towards a table on which they attempt placement of thoracic limbs) and obstacle courses.
The PLR and dazzle response can still be present in cases of central blindness and retinal disease.
Sudden vision loss can be due to subcortical or cortical disease. Subcortical lesions can affect the retina, optic nerve and optic chiasm. Cortical lesions occur in the optic tract, lateral geniculate nucleus, optic radiations or occipital cerebral cortex. (Platt et al, BSAVA Manual of Canine and Feline Neurology, 4th ed)
(Platt et al, BSAVA Manual of Canine and Feline Neurology, 4th ed)
Retinal disease includes sudden acquired retinal degeneration syndrome (SARDs), retinal inflammation and detachment, neoplasia, toxicity and infection.
Sudden Acquired Retinal Degeneration Syndrome
SARDs causes vision loss over days to weeks and typically occurs in middle-aged female dogs with Brittany Spaniels, Dachshunds and Miniature Schnauzers being over-represented.
SARDs is usually accompanied by polyuria, polydipsia, polyphagia, weight gain and hepatomegaly. Many affected dogs have signs indicative of hyperadrenocorticism however they often have normal or equivocal LDDT and ACTH stimulation test results. Clinical signs of Hyperadrenocorticism often resolve after a few months.
Ophthalmic examination of patients in the early stages of SARDs is usually unremarkable with a delayed PLR being the only sign of disease. Electroretinogram (ERG) testing however will reveal a ‘flat line’ ERG trace, this is pathognomic for the condition. Common differential diagnosis include retinal inflammation and central disease. The cause of SARDs is thought to be immune-mediated. There is no treatment for SARDs and blindness is total and irreversible.
Retinal inflammation and detachments
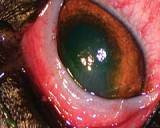
Retinal inflammation is associated with varying degrees of retinal change indicative of inflammation, some cases will appear normal. PLR may still be present as fewer axons are required for this reflex than are required for conscious perception of vision. The cause is suspected to be immune-mediated and treatment involves the use of oral corticosteroids. More than 50% respond within 7-14 days of commencing treatment, however cases can recur. Retinal detachment is usually clearly visible with ophthalmic examination. Optic Nerve lesions Optic neuritis causes acute and often bilateral vision loss. Any breed can be affected with Maltese being the most common. Pupils are dilated and there is no PLR reflex present. Fundus examination may reveal signs of optic nerve inflammation depending on the area of the optic nerve affected (in the eye as apposed to behind the eye). Aetiology suspected to be immune-mediated but an associated with granulomatous meningoencephalitis (GME) may be under-estimated. Other less common causes include canine distemper virus and cryptococcus infection. Where no underlying cause is suspected, oral cortisone is the treatment of choice, with approximately 50% regaining some vision in one or both eyes. An absence of response to cortisone may warrant further investigation such as magnetic resonance imaging (MRI) of the brain. The main differential diagnosis is papilloedema (oedema of the optic disc).
Optic chiasm lesions
Neoplasia at the optic chiasm results in decreased to absent vision. The pupils are dilated with no PLR reflex. Lymphoma is a common cause in cats, pituitary macroadenomas, meningiomas and extension of nasal cavity tumours should also be considered. Inflammatory and vascular lesions at this region will present with similar symptoms.
Optic tract lesions
Optic tract lesions result in visual deficits in the lateral visual field of the contralateral eye and medial visual field of the ipsilateral eye. As the menace response assesses the lateral visual field of the eye being tested, the response will be reduced or absent in the contralateral eye. PLR is intact in both eyes. Causes include GME, toxoplasma, cryptococcus, FIP, neoplasia or vascular lesions.
Central disease
Lesions affecting the central portion of the visual field result in visual deficits in the contralateral eye but the PLR is unaffected. Associated neurological signs (decreased consciousness, circling, proprioceptive deficits and hemi-neglect) are usually present in cases severe enough to cause visual deficits. Causes include degenerative disease (lysosomal storage disease), encephalopathy due to metabolic disease (liver shunts, renal disease, hypoglycemia, hypothyroidism), neoplasia (meningiomas and gliomas are common), GME and infectious causes as for optic tract disease, trauma and vascular disease. Global cerebral ischemia may occur as a result of hypoxia during general anaesthesia or after prolonged seizures resulting in persistent cortical blindness.
Sudden vision loss is a worrying clinical sign for owners and can present a diagnostic challenge. Thorough ophthalmic and neurological examination assists in localising the lesion however further diagnostic testing (ERG, blood tests and MRI) may be required to give a definitive diagnosis and prognosis.