Many ulcers in general practice can be successfully managed medically, and in some cases additionally with a temporary tarsorrhaphy or a third eyelid flap. However for deeper ulcer where perforation threatens then there is an indication for placing a graft to support the cornea.
This may be mechanical support or it may be for nutritive support. If the cornea has a deficit greater than 50% of its thickness then a mechanical support should be considered. A nutritive support graft usually does also increase mechanical support but is primarily used to deliver a blood supply to the cornea.
Conjunctival grafts
The conjunctival pedicle graft: This is usually used when there is a focal deficit in the cornea. It will deliver mechanical and nutritive support. The graft is opaque but can be trimmed later to an island graft to reduce the impact on vision (under topical anaesthesia).
Conjunctival pedicle grafts may be placed over tectonic grafts such as donor corneal buttons, fascia lata. These are need if the cornea is very thin and is bulging over a large area. The conjunctival grafts in these cases are not strong enough to provide corneal strength on its own. The conjunctiva can also be used as peripheral hood grafts and bridge grafts.
 Pedicile grafts.
Pedicile grafts.
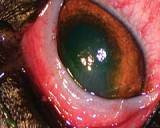
The 360 degree conjunctival graft: This is used when there is a large (in area) defect in the cornea. This is usually a salvage procedure and significant scarring is to be expected with such a large initial corneal lesion. Conjunctival 360 degree grafts are technically easy to do, and with the correct equipment a general practitioner should be able to do this graft. A second procedure under GA will be required to remove the graft. These grafts may save the globe but vision may not return due to the corneal scarring. 

Melting ulcer with spectacular hypopyon & 360 degree graft.
Acell Grafts
These grafts provide mechanical support alone to the cornea. Multiple layers of porcine bladder submucosa (“Acell”) can be placed in a defect and sutured in, generally with an overlying conjunctival graft. This graft provides a scaffold for invasion of stromal keratocytes to improve healing. They do not provide nutrition or immune response unless a conjunctival graft is used as well. Corneoconjunctival transpositions (sliding grafts) In these grafts we take neighbouring, healthy cornea and slide it over the defect, advancing the limbus with conjunctiva attached. This should clear over time so is a great technique for axial lesions as the limbal and conjunctival part of the graft remains peripheral thus giving a clear visual axis. This provides robust mechanical and some nutritive support as the limbal blood vessels are brought closer to, but not over the lesion.

Perforated ulcer in a pug (there is an area of axial pigment adjacent to the ulcer) & Same eye after a corneoconjunctival transposition
Corneoconjunctival transposition in a cat, 3 months after surgery.
Corneoconjunctival transpositions (sliding grafts)
In these grafts we take neighbouring, healthy cornea and slide it over the defect, advancing the limbus with conjunctiva attached. This should clear over time so is a great technique for axial lesions as the limbal and conjunctival part of the graft remains peripheral thus giving a clear visual axis. This provides robust mechanical and some nutritive support as the limbal blood vessels are brought closer to, but not over the lesion.
Conjunctival Grafts
In all grafts that are directly sutured to the cornea (Acell, Conjunctival pedicle and corneoconjunctival) the cornea to which it is sutured needs to be stable and non infected. The deficit may need to be enlarged by the trimming back to the healthy tissue required for suture retention. A 360 degree graft may be placed over unstable and infected tissue if required as it is sutured to itself. Infected/ melting corneas can be managed surgically by resection of the infected area and graft placement.
Sutures used in the cornea should be 8/0 or smaller and magnification should be used to improve technique. The conjunctival portion of any graft should be thinned as much as possible by removing the sub tenons layer (white layer under the conjunctiva). This layer contains contractile elements which will pull the graft off if not removed. The graft should be under no tension at the time of suturing so that the unsutured graft will sit in the defect without retracting. It is harder to prepare a graft in a flaccid eye so we usually take the graft (having assessed the size required) before addressing the cornea itself if the defect is at risk of perforation. Ideally the base of the graft should be either dorsal or ventral so that the eyelids run with the graft, rather than across it, when blinking.
Always be generous in the assessment of graft size required. Conjunctival grafts can be trimmed smaller if required but it is really annoying when they are too small and that is hard to rectify. We can be contacted on the VETLINE 9572 1966 at any time if you have a nasty cornea.