Is my pet a good candidate for cataract surgery?
Cataract surgery is an involved and intricate surgery. We need to make sure that your pet is healthy and is free of any problems that might interfere with the success of cataract surgery. In some older dogs we may recommend that your local veterinarian decided whether your pet requires a physical examination and preoperative blood & urine tests, and in some cases chest x-rays and heart examination.
Age alone is not a deterrent to cataract surgery. With the use of modern anaesthetic agents cataract surgery has been successfully performed on dogs and cats as old as 19. One concern with older dogs is that their retinas may also have age related degeneration. In some older dogs the surgery goes well, the eye is clear, the retina is healthy on ophthalmoscopy, but the vision is poor, and we suspect poor brain function in these cases. In some cases these older dogs can be treated with new drugs that help with senility.
Diabetic dogs make excellent candidates for cataract removal. The increased sugar levels in the lens make the cataract softer and easier to remove with the new technique of phacofragmentation. Diabetic patients can have problems as their wound healing is slower and they are more prone to infection. This is overcome by using more sutures to close the wound than we normally use, and by giving postoperative antibiotic tablets.
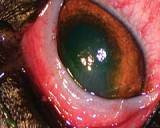
Cases in which there has been pre-existing reaction against the cataract (lens induced uveitis) tend to have poorer success rates. This reaction will increase the risk of more inflammation after surgery, glaucoma, retinal detachment, bleeding and cloudiness in the eye. We will assess your animal’s eye so we can give you an indication as to the expected prognosis.
When to operate
When is the best time to operate?
In the past cataract surgery was usually delayed until the cataract had matured and the patient had become totally blind. We now know that surgery is considerably more successful if the cataract is removed before it matures. We now decide to remove the cataract if it is likely to progress. This can usually be predicted by considering the animal’s age, breed, and the size and location of the cataract. In some cases the most predictable thing about cataracts is that they are unpredictable.
Caption: Cataract Machine with instruments
Allowing the cataract to grow and mature will reduce the success rate for a number of reasons. Firstly more mature cataracts are more likely to develop uveitis (inflammation) which can lower the success rate by as much as 20 to 30%. Secondly more mature cataracts can cause vitreous degeneration which may lead to cloudiness in the jelly of the eye. Thirdly the risk of retinal detachment is increased. Fourthly the capsule which holds the lens can become cloudy and opaque.
How is it done?
Surgery - How is it done?
Cataract surgery is performed using the latest proven technique of phacofragmentation. This is the same to what is presently done in humans. The surgery is performed with the aid of an operating microscope. A general anaesthetic is given, and a neuromuscular block is administered, which helps to improve access to the eye.
Ventilator Machine
Whilst under the general anaesthetic the animal is carefully monitored including measurement of blood pressure, and blood oxygenation by pulse goniometry.
Tubing a Dog Montioring Equipment Blood pressure probe Surgivet monitor
Two small incisions - the first being 1mm and the second 2.8 mm long - are made into the eye. The anterior lens capsule is removed with a fine pair of forceps. The cataract is then removed by phacofragmentation, which is ultrasound energy used to break down the cataract. In some cases part of the posterior capsule is removed. You can view this in the video below.
This video has been cropped. Subconjunctival Injection Sub conjunctival injection The incision in the eye is then enlarged to 8 mm through which the intraocular (artificial) lens is then inserted. The incision is then stitched closed with fine hair like dissolving sutures. Subconjunctival injections are given of Gentam (strong antibiotic) and Dexafort (cortisone). Laser is not used to remove the cataract - in humans laser may be used after surgery to remove scars, but it is not used to actually remove the cataract.
Removing cataract by phaco Insertion of a lens For these videos you will require some type of media player
Success & potential complications
Success and potential complications
Our success rate at Animal Eye Care is comparable to other veterinary eye specialists around the world. We regularly discuss and review our techniques with our colleagues both here in Australia and overseas. In young animals with early cataracts a success rate of over 93% is recorded. This means that for every 100 eyes we operate on, we are unable to restore vision in 7 of these eyes. We define success as the % of dogs having useful “guidance” vision. In cases where the cataract is mature and particularly those with pre-existing inflammation in the eyes, a much lower success rate is to be expected. We will discuss your pet’s situation so that you will have a good understanding of what the likely outcome will be. It is possible that if complications develop no vision at all will be restored.
With cataract surgery, both in animals and humans, there are a number of potential complications. These include glaucoma (increased pressure in the eye), uveitis (inflammation in the eye), cloudiness of the lens capsule, corneal oedema (a blue haze to the eye), retinal detachment, sudden retinal degeneration, and haemorrhages in the eye.
Causes
The most common causes of a poor vision following cataract surgery are
1) retinal detachment, which usually occurs 2 to 8 weeks after surgery;
2) severe postoperative inflammation;
3) glaucoma, which can develop hours after surgery or more commonly 1 to 3 years after surgery; and
4) scarring of the lens capsule.
It is very important to monitor the eyes after the cataract surgery. A number of studies have shown that the success rate drops off sometimes years after the surgery. We encourage eye examinations every 6 to 12 months after cataract surgery. We charge a fee for these long-term follow up visits. We are able to send out reminder letters to you.
Maximising success
Maximising the success
Carefully follow all of the pre- and post-operative instructions. If you are unsure at any stage please call Animal Eye Care at any time.
1) Elizabethan Collar: Train your pet before surgery to wear the Elizabethan Collar. It is important to restrict exercise/activity for 2 weeks after surgery, and very important to stop your dog from barking after surgery.
2) Laser Retinopexy: This recently developed technique can be used to reduce the risk of retinal detachment. The risk of retinal detachment is higher in certain breeds (such as the Bichon Frise, Boston Terrier and Poodle) and also if the eye is inflamed, if the cataract has been present for some time, and if the posterior lens capsule is accidentally ruptured or needs to be removed. In these cases we will recommend retinopexy to reduce the risk of retinal detachment. Retinopexy is done with laser surgery and it is where we 'weld' the retina onto the back of the eye. We often do this procedure with the ERG test, but can be done immediately prior to surgery. If problems arise during surgery, the retinopexy can be done immediately after surgery. Even with retinopexy it is still possible for the retina to detach, but the likelihood is reduced.
Laser Retinopexy Machine
Recovery
How long will my dog need to stay in hospital?
Dogs are admitted at 8am on the morning of surgery, and are discharged later that afternoon. Surgery is conducted in the middle of the day, but after surgery we need to keep a close eye on the dog's intraocular pressures (IOPs). We do not keep animals overnight as our clinic is unstaffed outside normal business hours.
We will need to see your dog the following day to check the IOPs again, and then generally several times in the following fortnight..
Prior to surgery
If we were unable to see the retina because the cataract was too cloudy, we will need to do an ERG to see how healthy the retina is. Starting 3 days before surgery cortisone drops are commenced. One drop of the Maxidex/Prednefrin Forte is given three times daily to the eye(s) being operated on, and Voltaren drops twice daily. We sometimes also start anti inflammatory tablets 3 days before surgery. These are usually given twice daily for 3 days before and 3 days after surgery, and then once daily.
Following Surgery
We send the dogs home with an Elizabethan Collar that will need to stay on for a week. This may cause some disorientation for the first 24 hours. We feel that this is a small price to pay to minimise the chance that the dog may accidentally damage the eye. You and your dog can be accustomed to the collar by having your dog wear the collar before surgery.
Generally there is little if any pain associated with the procedure. Most dogs settle down very quickly after the surgery. We routinely give a pain relieving injection on the morning of surgery and tablets are continued after surgery, so there is no need to give pain relief at home. All cataract patients are given an injection of Convenia (an antibiotic) which lasts up to 2 weeks.
Antibiotic drops will need to be given 4 times daily for 5 days after surgery. The cortisone drops which were given before surgery, are stopped for these 5 days, and are then usually given twice daily from day 6 after surgery.
Usually 4 to 6 weeks after surgery, the top of the eye may become a little red and blue. This is due to a reaction developing as the sutures dissolve out. This does not seem to be associated with any pain or discomfort. The cortisone drops will help reduce this reaction.
Post-operative visits
Your dogs eye will be examined a number of times the afternoon and evening of surgery. We need to recheck the eye the day after surgery then day 3, 10, and 24 after surgery. These visits are included in the surgery fee. We then suggest visits every 6 to 12 months to monitor the progress and health of the eye. A fee is charged for these visits. We consider these appointments very important to make sure that complications do not develop later on.
Vision after successful surgery
With the cataract successfully removed the dogs vision is greatly improved, and most dogs return to their previous activities. We routinely recommend that we replace the cataract lens with a plastic intraocular lens (IOL).
We find that with an IOL animals regain their vision much more quickly. The IOL also helps with their close-up vision and depth of field perception. An IOL also seems to reduce the risk of secondary lens capsule fibrosis from forming. Not all patients are suitable for an IOL. Without a lens after cataract surgery generally the patient's close up vision (less than 75 cms) is poor, but the mid to long distance vision is normal. Many dogs without a replacement lens seem to have useful vision.
As in humans it seems to take 3 to 7 days for the dog to regain useful vision. In some cases it may take up to 6 weeks for the dog to learn how to see again.
One or both eyes?
In humans only one eye would ever be done at a time. Most veterinary ophthalmologists are happy to do both eyes at the same time. There is a small risk that the surgery is not successful in both eyes if a complication such as an infection should develop. Fortunately this is very rare with the new small incision techniques of cataract surgery. The benefits of doing both eyes are that the surgery is substantially less expensive, and only one anaesthetic is required. The decision on whether to operate on one or both eyes is yours to make.
Future
Will the cataract grow back?
In the vast majority of cases no, as the entire lens protein that causes the cataract is removed. In very young dogs they can rarely have regrowth just in the edges of the lens. This is rarely a problem except in dogs under 12 months of age.
In some cases we can get cloudiness of the lens capsule, which can look like a cataract. We remove the anterior capsule, and generally leave the posterior capsule. In some cases it is possible for the capsule to become opaque, and this may look like a cataract. In most cases this does not seem to affect the dog’s vision, even though you may notice the cloudiness. In very rare cases we need to surgically cut out the cloudy scarred capsule. This problem seems to be most common in young dogs. For dogs under the age of five we routinely recommend removing the posterior capsule at the time of surgery. This will require us to do retinopexy to reduce the risk of retinal detachment, which can follow posterior capsule removal. In some cases we find that the posterior capsule is cloudy when we have removed the cataract, in these cases we will remove the capsule, and then do laser retinopexy immediately after the surgery is completed.